What is Glaucoma and How is it Treated?
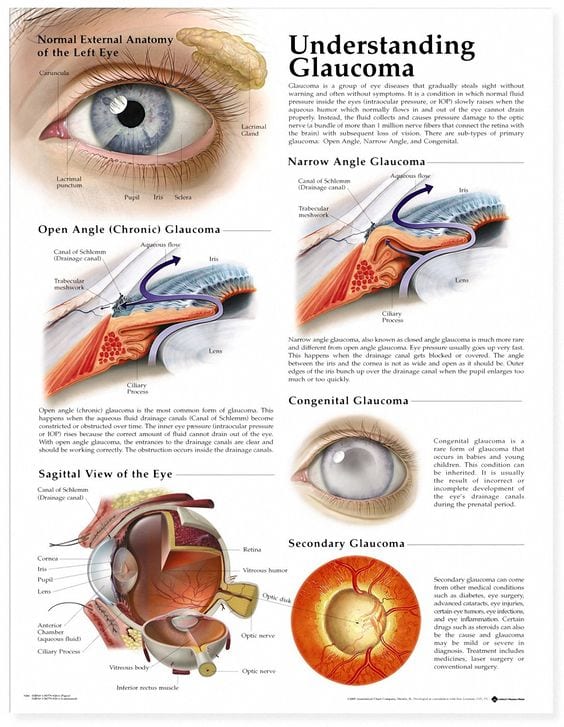
Glaucoma is a chronic disease defined by characteristic optic nerve damage. It is a complex and common disease, affecting over 40 million people worldwide. Glaucoma is a slowly progressive and irreversible disease and in most cases, causes a painless loss of eyesight.
The damage to the optic nerve is commonly caused by pressure in the eye, as well as possible decreased blood flow to the optic nerve. Lowering the pressure inside the eye can slow the process of optic nerve damage. The amount of pressure lowering that is necessary to prevent glaucoma from worsening is different for each person and each optic nerve. The more advanced the optic nerve damage, the lower the pressure needs to be to prevent further optic nerve damage and vision loss.
What Treatment Option is Right for You?
Your doctor has diagnosed you with glaucoma and has informed you that if it not treated, you may experience vision loss and eventual blindness. Commonly, eyedrops are used as a first line of treatment. In many situations, multiple medications are tried to achieve the desired pressure level. However, there can be difficulties with using eyedrops and laser therapy is commonly substituted as a first line of therapy. There are other alternative treatments available, but they generally have higher potential risk.
Recently there have been significant advances to better control the pressure inside the eye. Micro-invasive glaucoma surgeries (MIGS) involve bypassing the normal pathway for fluid to leave the eye. MIGS, including the iStent, CyPass, Xen®Gel, Kahook Dual Blade (KDB), and the OMNI are surgical therapies for patients who have mild to moderate open angle glaucoma. These surgeries are designed to improve the outflow of fluid from the eye, lowering the pressure inside the eye and reducing the need for glaucoma eyedrops. This helps reduce the risk of future vision loss from glaucoma.
Istent® and CyPass are implants that are placed in the drainage area of your eye at the time of cataract surgery. The implants stay in the eye to allow for lower pressure.
KDB and the OMNI are not implants, but are used to open up the drainage system in the eye to allow for lower pressure. These may be performed on its own or at the time of other eye surgeries.
Your surgeon will determine which one of these devices is best for you and your eyes.
All of these options are elective procedures. As your surgeon has discussed, these procedures are potentially beneficial in helping to lower the eye pressure and reduce the number of glaucoma medications that you take. If you decide not to have this procedure, other treatment options may be recommended and should be discussed with your physician to better control your glaucoma.
Anesthesia for MIGS Surgery
The iStent®, CyPass, Xen®Gel, KDB, and OMNI are are all performed through the same incision that is used for cataract surgery. In the case of the KDB and OMNI, a similar incision would be made, although cataract surgery does not need to be performed. An anesthetic agent is placed inside the eye just as is done in cataract surgery. The risks of anesthesia with cataract surgery are reviewed in your cataract surgery informed consent.

Risks and FAQ about MIGS
Microinvasive glaucoma surgeries successfully lower the eye pressure in most cases. However,sometimes this may not be sufficient to stabilize your glaucoma. In some cases, the procedure may not function well at all, even though the surgery as been performed properly. There is a higher risk of bleeding inside the eye from these procedure; this bleeding may blur the vision but typically will clear up within a few days after surgery. There is additional risk of the CyPass implant (but not the other procedures) causing the eye pressure to drop too far or cause the eye’s focal point to be different than what is expected from the cataract surgery (more nearsighted than expected). These complications typically resolve on their own with time. It is possible that the CyPass® or iStent® would need to be removed if they are causing persistent problems. It has also been noted that the CyPass can cause damage to the inside layer of cells of the cornea if it is not in its correct position. This can potentially cause clouding or swelling of the cornea and require treatment, possibly including a corneal transplant. In addition, sometimes there can be complications that do not appear early on but may develop days, months or years later. You may need further treatment or surgery to treat those complications. As with any intraocular surgery, there may be loss of vision, blindness, loss of the eye, as well as bleeding, infection and injury to the eye or nearby body parts.
These procedures should not be performed in eyes with angle closure glaucoma, including uveitic (inflammatory) glaucoma. They should not be performed in patients with neovascular glaucoma or in patients with thyroid eye disease, Sturge-Webber syndrome or any other type of condition that may cause elevated episcleral venous pressure.
Am I a candidate for MIGS?
Only a thorough and comprehensive consultation and evaluation of your open angle glaucoma with an experienced ophthalmologist will determine MIGS candidacy. To schedule a consultation with Dr. Shatz or Dr. Shield, please contact our office through our website, or call 413-584-6422.